BY LISA SIMMONS-FIELDS, DNP, MSA, RN, CCM, CPHQ
Objectives: Increase care management engagement, education, retention and decrease turnover.
Background: Transformational nurse leaders have the capacity to influence the professional competencies and engagement of the care management teams.
Methods: The project design is a prospective, mixed method design.
Results: Team response and early trends are positive for increased engagement and decreased turnover.
Conclusions: Continued research is recommended to develop sustainable strategies to prevent healthcare worker exodus.
Introduction
Care management leaders can strongly influence care management turnover and retention, thereby influencing care delivery across the care continuum improving safety and the quality-of-care delivery.
As part of our investment in the professional development of our ambulatory and practice-based care manager nurses and social work teams, Trinity Health has collaborated with the Case Management Society of America (CMSA) to provide training through their Integrated Case Management program. Integrated care aligns with Trinity Health’s commitment to whole-person, personalized care for life by developing trusted patient relationships.
Trinity Health, as a large national Catholic healthcare system, understands the importance of accepting who each person is: a unique individual with a unique story. The underlying causes of a condition can be much more than condition burden or symptoms. Social needs and untreated or undertreated conditions are common contributors to poor health.
Care managers trained in an integrated approach assess risk in the four domains of health: biological, psychological, social and health system. They use these assessments to develop and create a shared person-centric plan of care. The ICM training provides advanced assessment training, identifies the person’s experiences, concerns and what is contributing to poor health. This results in a plan of care that focuses on what is most important to the person.
Trinity Health’s commitment to continuous learning and personalized care delivery supports our mission of being a transforming and healing presence within the communities we serve. To ensure we deliver high-quality, cost-effective care, we need highly engaged clinicians, consistent clinical practice and resources to deliver an exceptional customer experience. Our patients/members are the center of our care, and partnership throughout the continuum helps ensure our members achieve their health goals.
Purpose
The purpose of this quality improvement initiative is to determine whether additional care management education and membership in a national organization (CMSA) would improve onboarding, orientation, ongoing education and competency. Additionally, the goal is to increase retention and decrease turnover within our ambulatory care management teams.
Problem Statement
The ambulatory care managers needed a different solution for onboarding, orientation and ongoing training to ensure competency. Care managers are key members of the care team, supporting member care, transitions of care, care coordination, education and are well-positioned to improve the member experience, decrease cost and improve outcomes.
Prior to the implementation of the CMSA ICM program in April 2021, system data showed 31 new hires over the last 16 months, with 14 care managers (CMs) identified as having less than one year experience as a care manager. The health system cost of turnover is calculated as equivalent to a 12-month CM salary to train inexperienced staff. To ensure that we are the employer of choice, we need to recruit high-quality applicants and effectively train and retain our CM nurses and social workers.
Literature Review
Nurse retention is a significant challenge worldwide across care settings, with many nurses considering leaving the profession. Healthcare organizations and leaders need to apply strategies and tactics to retain their most valuable assets, their employees. Major themes identified by Dura and Hammoud, are “effective communication, respect, competitive financial compensation, benefits, and proper recognition.” Giving staff a voice, ensuring staff welfare and workforce planning support ongoing staff engagement.
A systematic review of leadership practices and staff nurses’ intent to stay supports the importance of a “positive relationship between transformational leadership, supportive work environments and staff nurses’ intentions to remain in their current positions” (Cowden, Cummings, Profetto-McGrath, 2011). Nurse leaders who ensure workplace environments that support quality and have strong relationships with staff were able to influence staff retention.
Doody and Doody (2012) discuss the importance of having transformational leadership that influences, inspires and motivates, ensures intellectual stimulation and provides for individual consideration. Effective leadership affects job satisfaction and employees are interested in working for leaders who can lead in a positive and encouraging manner. When job satisfaction improves, there is a ripple effect of patient satisfaction and retention.
Interventions
CMSA is a known entity for ambulatory care management. CMSA’s philosophy is aligned with Trinity Health’s in achieving goals for improving health outcomes for the population’s services. Training and membership in this professional organization provides an investment in our CM staff to grow and ensure ongoing professional competency. Highly trained and competent staff support being successful in advanced alternative payment models.
The Integrated Case Management Program (ICM) training includes guiding principles and practice expectations. The ICM program teaches care managers how to engage members, create trusted relationships, and perform a comprehensive assessment providing whole person care and the development of a care plan. “The ICM method supports the requirements of CMS to complete a comprehensive assessment, develop an individualized care plan, participate in interdisciplinary care team activities, and facilitate improved care transitions, and the patient-centered care approach support by an interdisciplinary team needed for success regardless of health setting” (CMSA, 2020). The CMS requirements pertain to other payers’ programs as well.
Each ambulatory care manager including nurses and social workers along with their leaders will receive the ICM training and have CMSA membership, providing access to CMSA library, tools and webinars. Care managers collaborating with complex patients will follow five patients for 12 months, record baseline ICM risk scores and provide quarterly updates on risk scores for the Medicare Shared Savings Program.
Project Aims
The aims of this quality improvement project were to
Increase competency and skills by training 90% ambulatory care managers and their leaders through the Integrated Case Management course by June 31, 2023
Increase access to educational events and training tools through the CMSA membership library
Decrease ambulatory care manager turnover rates
Increase the retention of ambulatory care managers
Theoretical Framework
The Neumann system model provides a frame of reference for evaluating and addressing health conditions across distinctive settings. The model supports a holistic framework supporting the use of clinical tools to guide assessment of individuals, families, communities and organizations to influence clinical practice. “Nurses evaluate the effectiveness of their interventions based on the degree to which clients met their goals” (Whetsell, Gonzalez, & Moreno-Fergusson, 2015). The ICM model provides for a standard way to identify health risks and health needs using the biological, psychological, social and health system domain. Through the evaluation of historical, current state and vulnerabilities, the CM can better identify areas of risk and priorities when developing a patient-centered care plan.
Method/Project Design and Interventions
The quality improvement project is a prospective, mixed model including self-study and interactive face-to-face virtual training. The program provides multiple strategies to engage patients, stratify risk and develop a patient-centered care plan to decrease risk and improve well-being. The interventional design included pre-work of reading the CSMA ICM book, 3-4 hours of online presentations and three four-hour (half-day) training sessions. Each cohort had a maximum of 20 people to ensure time for individualized and group interaction in reviewing case studies. The audience included a combination of nurses, social workers and CM leaders from the ambulatory care management teams that support the advanced payment models in the clinically integrated networks across the country.
Data and Analytics
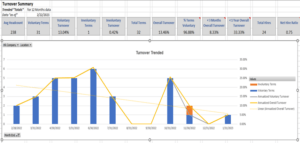
The turnover data trends for the ambulatory care management teams include a 12-month look back. The percentage of staff turnover within less than one year of recruitment is currently at 33% with a total of 24 hires of less experienced care managers. As noted in the graph, we have significantly decreased our turnover rates since the beginning of this intervention in June 2022. The overall turnover rate is 13.46%. The predominate reason sited for turnover was personal reasons and new jobs.
The initial retention trend includes a seven-to-eight month look back identifying colleagues who participated in the training in June through July 2022 cohorts, sessions 1-6. As noted in the table below, there is a 96.1% retention rate for these cohorts.
Conflict of Interest and Permissions
There are no conflicts of interest. The QI project aligns with the Catholic health system mission, vision and strategy and supports patient-centered relationship-based care through assessment and patient engagement leveraging motivational interviewing. Providing evidence-based learning opportunities for care management leaders and colleagues promote safe care and continuous quality improvement.
Limitations
Limitations include the timeline of the intervention and the need for continued monitoring and evaluation. There are three clinically integrated networks (CINs) that were not included in the turnover and retention graphs from the System Office Human Resource data. We have one region that will be attending the cohorts in April 2023.
Summary and Conclusions
Overall, the team was very appreciative of the CMSA ICM training. Quotes include “Today’s training was AWESOME! Becky is a wealth of knowledge and the question-and-answer activity about motivational interviewing was very good! I loved hearing the ideas and learning new ways to respond to patients in a way that inspires them and helps them to succeed. I certainly did not expect to enjoy this as much as I am.”
Creating team expectations and building upon knowledge and skills support our goal to continue to advance CM engagement and competency. Leveraging a system approach facilitates overall improvement in interventions, care plans and patient care delivery.
Continued quarterly monitoring of turnover and retention rates is recommended to monitor trends and ensure sustainability. The care managers are currently capturing patient risk scores based on the ICM-CAG model to determine baseline and every 3 months over a period of 12-months. The goal is to evaluate the efficacy of the CM interventions and decrease and/or mitigate risk.
Acknowledgments
The author thanks Rebecca Perez, MSN, RN, CCM; Michele Lee, Amy Black, Tom O’Grady, Sheila Johnson, MBA, RN; Emily Brower, MBA; Gay Landstrom, PhD, RN, NEA-BC, FACHE; Libby Edwards, Michelle Fitch and the CM Leaders and national teams for their commitment and support of the training and quality improvement initiative.
References
Cowden, T., Cummings, G., Profetto-McGrath, J. (2011) Leadership practices and staff nurses’ intent to stay: a systematic review. Journal of Nursing Management 19(4):461-77. doi: 10.1111/j.1365-2834.2011.01209.x
Doody, O. & Doody, C.M. (2012). Transformational leadership in nursing practice. British Journal of Nursing 21(20):1212-4, 1217-8. doi: 10.12968/bjon.2012.21.20.1212.
Duru, D.C., & Hammoud, M.S. (2022). Identifying effective retention strategies for front-line nurses. Nursing Management, 29(1):17-24. doi: 10.7748/nm.2021.e1971.
Fraser, K., Perez, R., Latour, C. (2018). CMSA’s integrated case management: A guide for case managers by case managers. Springer Publishing Company.
Whetsell, M. V., Gonzalez, Y. M., & Moreno-Fergusson, M. E. (2015). Models and theories focused on a systems approach. In J. B. Butts & K. L. Rich (Ed.), Philosophies and theories for advanced nursing practice 1st ed., pp. 407-434). Jones and Bartlett Learning.
Lisa Simmons-Fields, DNP, MSA, RN, CCM, CPHQ, serves as the director, System Population Health/Care Management for Trinity Health System. Lisa’s passion is standardizing evidence-based integrated care coordination programs to support the highest quality patient care.
Lisa serves as president-elect and chair of the Education and Membership Committees for CMSA-Detroit Chapter and the Editorial Board of CMSA. Lisa also serves on the Epic Care Management Advisory Board.
Image credit: ISTOCK.COM/DESIGNER491
The post Sustainable Strategies Related to Prevent Healthcare Worker Exodus: A Quality Improvement Project for Leaders appeared first on Case Management Society of America.
Source: New feed
